Nothing defines the unique character of George Clinical more than the people who do the important work of researching treatments and clinical practices that will shape medical policies and practices in every corner of the world. While our Scientific Leadership Team members are a diverse group from many countries and therapeutic areas, one thing they all share is a passion for making an impact on the treatment, and thus the lives, of the patients they serve. These are their stories.
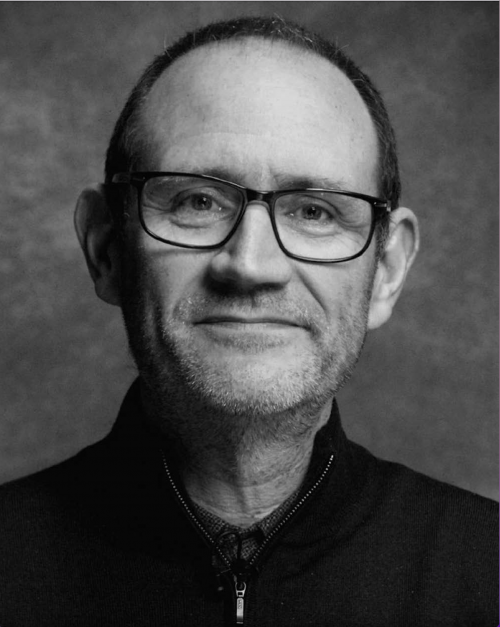
Professor Barratt’s research is focused on pathogenesis of IgA nephropathy and a range of areas across renal medicine including glomerular disease, multi-system renal disease and complications of chronic kidney disease, in particular renal associated anaemia. He is the IgA nephropathy Rare Disease Group lead for the UK National Registry of Rare Kidney Diseases and leads the Renal Research Group within the College of Life Sciences, University of Leicester. He also participates in other IgA nephrology initiatives such as the International IgA Nephropathy Network and in workgroups identifying endpoints for clinical trials such as the FDA and ASN Kidney Health Initiative.
Professor Barratt has been Principal Investigator for international randomized controlled clinical trials in IgA nephropathy and has attended both the FDA and EMA as an expert witness for new therapies in IgA nephropathy. He is an Editorial Board member for Kidney International and the American Society of Nephrology Journals and co-chairs the UK Glomerulonephritis Clinical Study Group.
I do think there is a challenge coming in terms of new approved therapies and recruitment to clinical trials in the traditional format, and there is a lot of effort at the moment to keep patients in ongoing trials. The challenge now is very much concentrated in the US because these new drugs are approved first in the US and become available first to patients in the US. But of course, over time, more and more countries will have these drugs available which will bring an increasing challenge. We need to think about how we design and deliver clinical trials now that we have new therapies coming thick and fast in this disease.
And this is about educating clinicians. If they want to start patients on these new treatments—start them early, and then assess whether a patient should be eligible for a trial. What we don’t want, is for patients to start these new drugs halfway through a trial. We also need to educate our investigators that if they delay starting one of these new drugs by two or three months, it’s unlikely to negatively impact on the patient’s long-term outcome, but could have a major adverse effect on the integrity of the clinical trial.
So, it’s very much about educating the clinical trial teams, about the suitability for bringing someone into a clinical trial where there’s a placebo control, and it’s about working with the sponsors to ensure that we match the clinical trial design with what is changing in standard of care therapy. It’s going to be a slow transition and we need to make sure trial design in IgA nephropathy moves with the times.
Undoubtedly the way we’re going to manage these diseases is with multiple therapies. We don’t have any trials of those combination therapies, and we need to be thinking about moving to trials of combination therapies in diseases like IgA nephropathy. That comes with challenges. But I think over the next three to five years we definitely need to explore different combinations of new drugs to gain the greatest benefit for our patients. What is clear is that many of the drugs currently in development for IgA nephropathy may also be useful in other forms of kidney disease and we need to explore what new indications there might be for these new therapies. Most sponsors do want to explore other indications for their drugs but are limited in their ability to deliver multiple simultaneous studies and so they have to, by necessity, deal with one indication at a time and then move on. That clearly delays the movement of a drug into different disease areas. But I’m sure that will come.

We have a massive growth in clinical trials of complement inhibitors, and these are going to be relevant to a whole range of different inflammatory kidney diseases. We are currently also evaluating a new class of drugs that target B cell modulation by inhibiting BAFF and APRIL. I think these drugs are equally relevant in other antibody mediated kidney diseases. I’m sure once we start seeing some of the data in IgA nephropathy, we will see these drugs move into other areas, such as lupus nephritis, membranous nephropathy, ANCA-associated vasculitis—lots of opportunities.
There are already combination trials in progress looking at the combination of renin-angiotensin system blockade, SGLT-2 inhibition and endothelin receptor antagonism for treating chronic kidney disease. What we would like to see are trials of combination therapies targeting the immune system in IgA nephropathy.
We need to be evaluating drugs in as diverse populations as possible. That’s because we need to understand how a drug works in populations with different genetic backgrounds and in different parts of the world. There are clearly differences in the way diseases behave in different populations. For example, in people of East and Southeast Asian origin, IgA nephropathy is more common and is more likely to put you on dialysis. We don’t understand why that is. There may also be environmental factors that can influence drug efficacy and drug safety.
We need to ensure we offer the opportunity for clinical trial involvement to all patient populations, including those disadvantaged populations in all parts of the world—women, children, people of different races, people at different levels of social deprivation. We need to work hard to ensure that we reach those populations, and that we are able to give them the information they need to feel safe and confident about being involved in research.
Patient engagement starts from the very beginning—at the protocol stage—before the trial design is finalized. It’s about listening and understanding. Patients say things that as clinicians and researchers, we may not have thought about. They have a lot to offer in terms of talking through the type and frequency of procedures they’d be prepared to have as part of a clinical trial. They can review the information sheets that are given out to patients to make sure they are readable and understandable. They can help us learn what would make the trial easier for a patient—like frequency of visits, home nursing and sample collection. All of these things are really important in making sure that a trial is designed with the patient at the center of the process.
This is the responsibility of the entire clinical trial team including the sponsor, the CRO and the local site staff. I have experience of studies where this wasn’t really thought about, and I think they have suffered because of that.
I think George Clinical has a clear renal pedigree. They have established a global network of highly credible, highly experienced nephrologists with proven track records in the design and delivery of clinical trials in both common and rare kidney diseases. They’ve shown they can work collectively as a team, and that they can deliver clinical studies exactly as planned with high quality data. The network and relationships that George Clinical has developed over the many years that they’ve been in the renal space has been integral to the success of the trials that they’ve been involved with.
What we have now is a global network of nephrologists who have delivered clinical trials and want to deliver more, and they know how to do it. Seeing these studies published in high profile publications—new drugs getting approved for our patients—justifies all the time and effort spent in delivering these clinical trials and really changes clinical practice for the better. This applies to the whole research team. Success breeds success, and sites have the confidence that they can deliver kidney studies.
To the FDA it would be to keep their innovative approach to assessing drug efficacy in rare kidney disease. They have been true trailblazers in facilitating drug development in rare kidney disease and they need to continue to challenge themselves to see whether the endpoints we are using at the moment can be refined. The FDA are engaging with nephrologists to explore opportunities so watch this space.
To pharmaceutical companies, I think the key message is to keep investing in kidney disease, and in particular rare kidney disease, and keep working with the experts to get the advice and guidance they need to make sure that their programs are a success.
The entire nephrology community is to be congratulated for stepping up to the challenge of delivering global trials in rare kidney disease. But we need to make sure that everyone understands that the job is not done. We have to continue to deliver these trials because we are going to need more therapies than we have at the moment to prevent kidney failure in our patients with rare kidney disease.
Family time is important, and I like listening to music, especially blues, country and bluegrass. We’re going on our family holiday to Nashville this year with plans for the Ryman and the Grand Old Opry. And I like watching sport—rugby and football (the original, and best, version!).
ASN Kidney Week 2023: Signaling the Onset of a New Golden Age for Kidney Disease Clinical Trials